DEPRESSION
Illness and not a weakness of character
Everyone goes through ups and downs. Often there are reasons for a bad mood, e.g. incisive life events such as the loss of work, grief or conflicts with other people. Usually, people recover from such in the foreseeable future. However, when the bad mood manifests over weeks and months and increasingly begins to influence daytime activities, social relationships, or work performance, depression can develop.
Depression is a disease that affects people on a physical and psychological level and thus in their entire thinking and experiencing. It affects not only the ability to work, but also family and social relationships. The behavior of those affected changes.
The World Health Organization (WHO) has compiled criteria for the diagnosis of clinical depression and accordingly certain depressive symptoms must prevail for at least two weeks
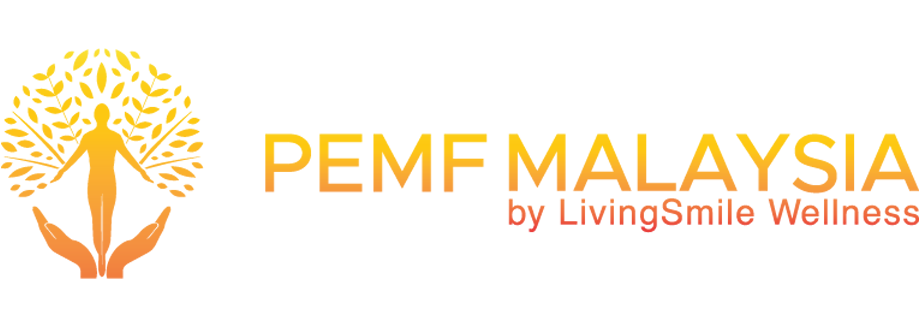
The three main symptoms are:
- Gloomy or depressed mood
- Loss of interest and joylessness in activities that were otherwise enjoyed
- Lack of drive and increased fatigue
Other symptoms:
- Decreased concentration and attention
- Decreased self-esteem and self-confidence
- Feelings of guilt and worthlessness
- Negative and pessimistic future perspectives
- Suicidal thoughts and attempts
- Sleep disorders
- Loss of appetite and weight loss
- Loss of Libido
- Internal restlessness or lack of drive
The more symptoms that prevail and the more pronounced they are, the more severe the depression is. The composition and severity of the symptoms can vary greatly from person to person. The treatment must be adjusted accordingly and individually.
Possible Symptoms of Depression
How common is depression?
Depressive diseases are among the most common mental illnesses. The lifetime prevalence of depression is approximately 17%. This means that 17% of the population in life experiences at least one depressive disorder. Women are affected more often with about 20% lifetime prevalence than men with about 13%.
The WHO estimates that in 2030 depression will be the most burdened affliction, before cardiovascular disease.
How long does depression last?
Depression usually occurs in episodes, followed by depression-free periods with partial or complete absence of symptoms. A depressive episode lasts on average between half a year and one year, until the mood returns to normal spontaneously. As a consequence, antidepressant treatment should last for up to one year, even after a good improvement in symptoms.
Most people experience multiple depressive episodes that can occur at different intervals. The more depressive episodes someone has already experienced, the greater the risk of experiencing another episode. Despite this episodic course, one speaks of depression as a chronic disease.
MANIFESTATIONS
The type and severity of symptoms of depression can be very different from person to person.
More common forms of depression are listed following:
• Unipolar courses
• Bipolar courses : Patients not only experience depressive episodes but also manic episodes in between. Manic episodes are characterized by an unrestrained thirst for action, an upscale mood, a lack of sleep, size ideas that often lead to a shopping spree or start of over-ambitious business projects.
• Seasonal Depression : Dark and foggy winter days can worsen the mood. The cause is the seasonally reduced incidence of light through the eye and possibly a shift in the circadian rhythm. Light therapy is a common treatment of winter depression.
• Late-life depression : People over the age of 65 years are generally referred to age depression. Significant life events, loss of relatives or friends, serious illness or financial problems become more important in old age as risks of depression. Overall, however, depressive illnesses in older age do not occur more frequently. Cognitive disorders in the context of age depression are often indistinguishable from incipient dementia.
• Postpartum depression : Depressive postpartum episodes due to rapid hormonal changes occur in approximately 10-15% of women and usually begin in the first or second week after delivery.
• Men’s depression : In some people, the depression may also be due to irritability, aggressiveness or increased alcohol consumption. Under certain circumstances, a lot of sport is done. Those affected feels stressed and burned out. Men are more frequently affected by these types of symptoms.
• Dysthymia is a creeping, chronic type of depression with the same symptoms as a depressive episode. The symptoms are less pronounced, but they last a very long time.
RISK FACTORS
Family burdens and the genes
There are familial accumulations of depression which indicate a hereditary, increased risk of this illness. However, it is not the disease itself that is inherited, but the increased risk of responding to prolonged stress with depression. The cause of this increased, familial risk of depression is hardly a single “gene of depression”, but a whole number of genetic variants, which in their interaction result in increased susceptibility.
Such gene variants play a role not only for the susceptibility and individual expression of depression, but also for drug therapies of all kinds. For the pharmacotherapy of depression, for example, gene variants that control the rate at which drugs metabolized in the liver or their ability to reach their place of action play a role. It is to be hoped that the research will soon be able to provide further knowledge, which enables individually tailor-made therapies – in the sense of “personalized medicine”.
Early childhood experiences
In addition to familial accumulations, it has been shown that stress experiences, especially in early childhood, increase the risk of mental illness, especially depression and anxiety disorders.
This is a phenomenon called epigenetics. This includes a level of regulation which is superordinate to the actual genes. For example, changes in the DNA determine whether a particular gene is active, that is, frequently read or muted. As we now know, environmental influences – such as early childhood stress – can lead to such epigenetic changes.
History of depressive episodes
The risk of developing new depression continues to increase with each relapsed episode, especially if residual symptoms of an earlier stage persist, such as sleep disorders, lack of concentration or lack of energy and initiative. It should, therefore, be stressed out that depressive episodes should be treated consistently and long enough until all residual symptoms have been overcome and the patient has regained full functionality.
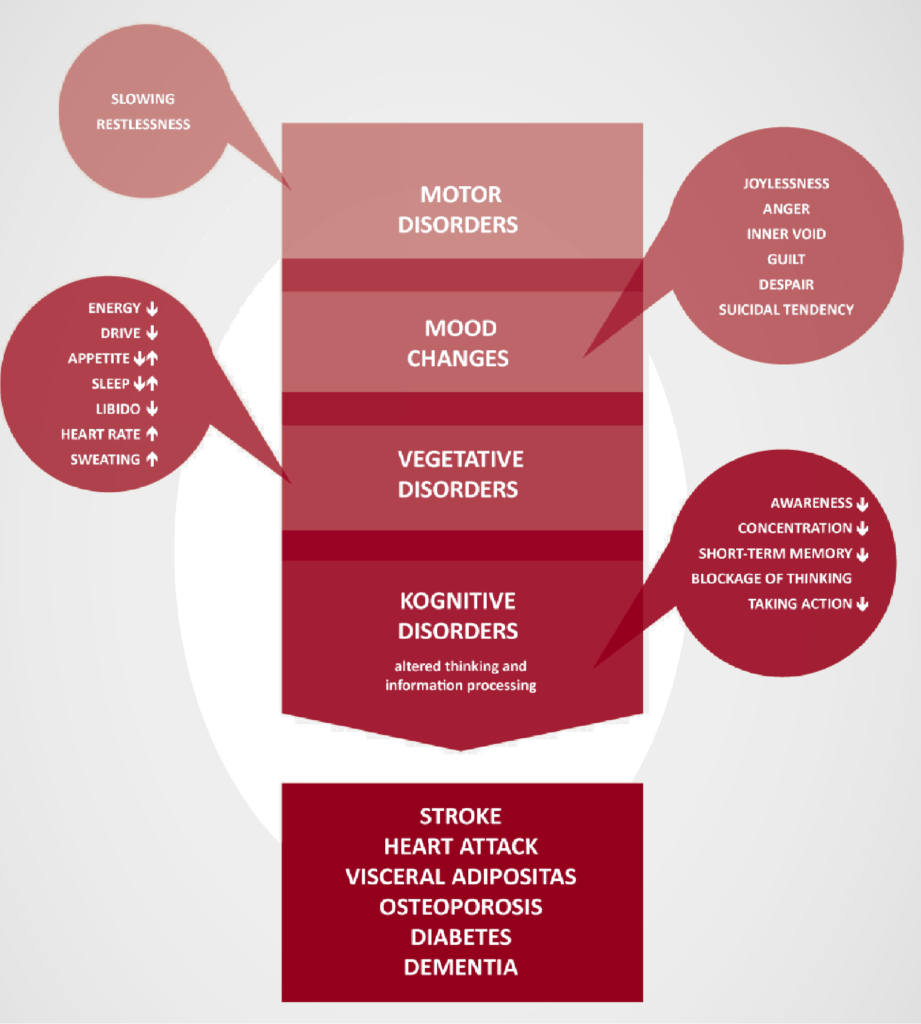
STRESS AND NEUROBIOLOGY OF DEPRESSION
Research has shown that depressive patients have altered blood cortisol levels. Cortisol is a typical stress hormone, which is released especially in case of excessive demands and feelings of loss of control. Depression is therefore increasingly seen as a stress disorder.
Stress hormones and depression
Our body reacts to every external and internal stress with mental and physical reactions, be it a short-term sportive challenge, a brief noise pollution or longer-term stress situations such as a high workload or ongoing social conflict situations. Challenges that allow for active and successful coping can trigger positive emotions, even though (or because) stress hormones like epinephrine and norepinephrine are released and positive energy is mobilized. This type of stress reaction is only of short term and called eustress.
On the other hand, long-lasting stressful situations that lead to excessive demands and loss of control cause and establish negative feelings and thinking patterns with high levels of the stress hormone cortisol. In certain brain regions, the so-called limbic system, which is responsible for the regulation of our emotions, this leads to overactivity of the amygdala. On the hormonal level, there is a pathogenic, permanent activation of the stress hormone system (hypothalamic-pituitary-adrenocortical system). The brain loses control of the stress hormone system that is no longer at rest and constantly firing.
When internal and external stressors exceed the individual coping abilities, stress becomes harmful.
The negative individual experience and processing of stressful events can lead to depression
Brain and Depression – Untreated depression changes the brain
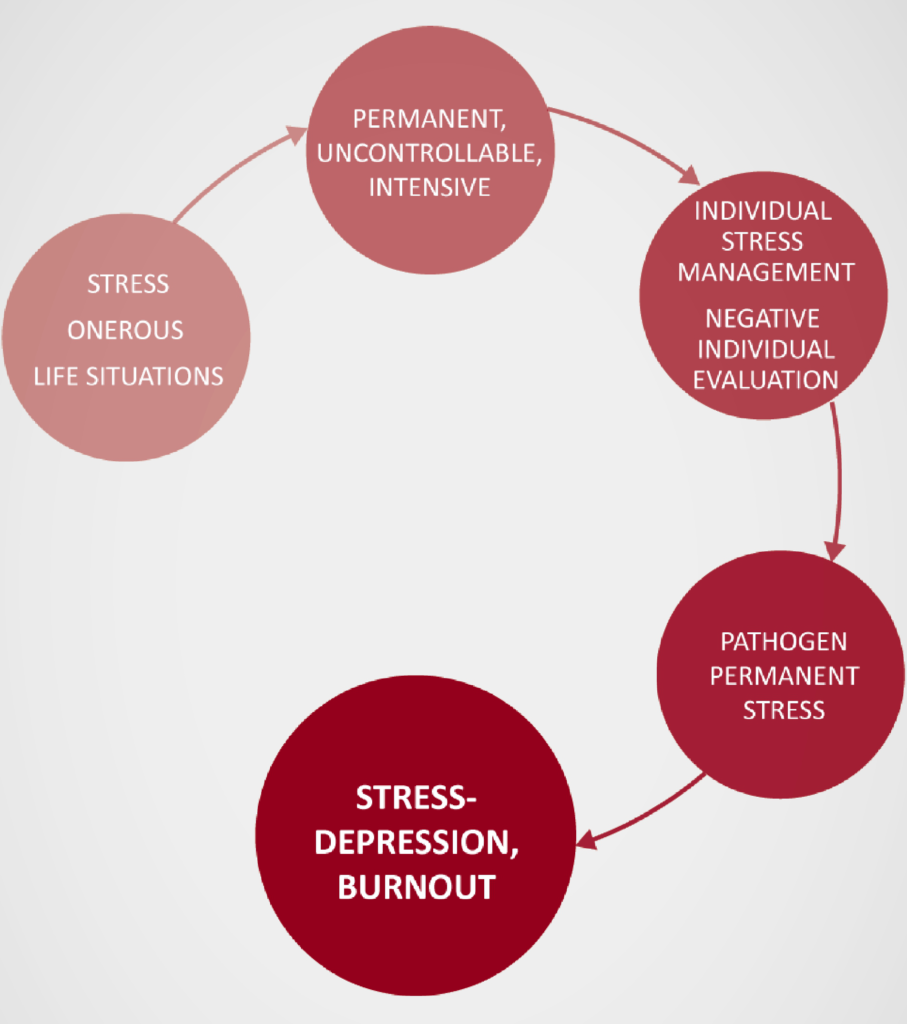
It has been known for some time that the metabolism of messengers like serotonin, norepinephrine and dopamine is altered in individuals with depression. At the contact points of the neurons in the brain, the synapses, the stocks of these transmitters are exhausted, so that the transmission of information from neuron to neuron is disturbed. These events are directly related to the above-mentioned overstrained stress systems.
Depression can arise and be treated both physically and biologically as well as psychologically and psychosocially. All of these causes, be they innate or environmental, can lead to chronic stress and pathological overactivity of the stress hormone system. Result of this overactivity is a disturbance of neuronal metabolism.
Recent findings in depression indicate that the formation of new neurons in the limbic system is reduced or even suppressed. This inhibits the natural ability to regenerate these brain areas, which are of central importance for feelings, stress management and learning ability. If depression is not treated for a long time, it could even be shown that these brain areas decrease in volume and become smaller. This is mainly due to the negative effect on the brain of chronically high cortisol levels.
The latest findings show all the more that the complex disease must be addressed and treated holistically. This is done by an individually optimized combination of psychotherapy and drug therapy, as well as appropriate accompanying measures (sports, group therapies, self-help or, for example, the application of PEMF). The concept requires a non-stigmatized understanding of the disease and openness to all available treatment options.
TREATMENT AND THERAPY
Depression is a very complex disease. It is still often fraught with feelings of personal failure, ignorance and stigmas. Properly treated, depression today is often curable. However, effective and well-tolerated treatments are still frequently not used, as depression is overlooked and underestimated in severity. Even if depression is recognized, only less than half of these patients receive consistent, antidepressant treatment. There are several reasons for this, whether because no effective treatment has been prescribed, or because patients do not comply with or stop treatment prematurely out of fear or lack of education for the use of antidepressant drugs or decline the offer of psychotherapy.
The goal of any antidepressant treatment must be full recovery in order to give the patient an unrestricted life again. Curing depression takes time and patience.
Several international and national associations have developed treatment guidelines that are based on the latest knowledge of all available therapy options for depression. These not only describe different treatment algorithms for customized therapies, but also give instructions in case of insufficient or missing response, the necessary duration of therapy and prophylactic treatments in persons with a high risk of relapse.
Basically, an antidepressant therapy is divided into the three time periods: Acute therapy (first 6-12 weeks), Maintenance therapy (4-9 months) and a possible relapse prevention (longer than one year).
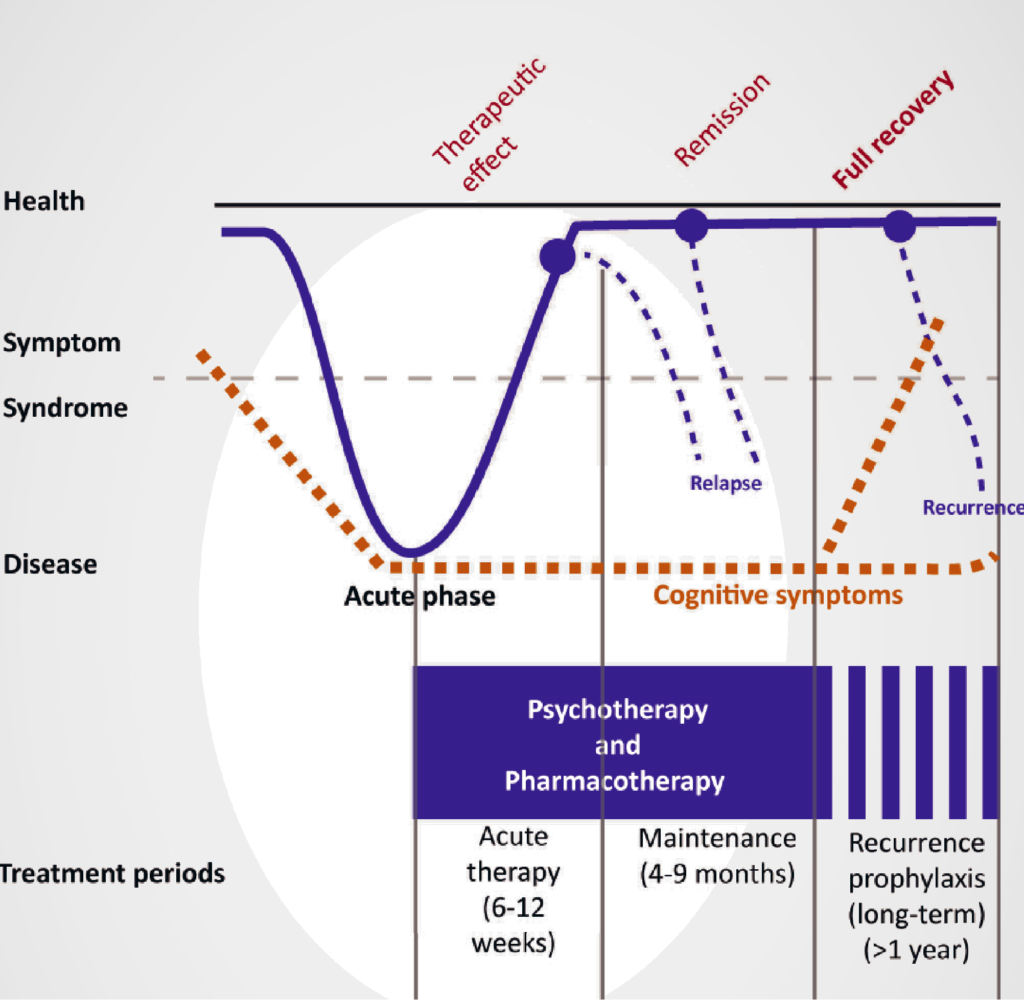
The different sections of successful treatment and relapse prevention
Psychotherapy
The adequate treatment of depression must always include psychotherapy. Since each patient has an individual emotional profile, a treatment tailored to each one of them is required. This ideally leads to a change in stress management and to the correction of negative individual evaluation and processing of stressful life events. In psychotherapeutic procedures, cognitive-behavioral therapy (CBT) and interpersonal psychotherapy (IPT) are currently best studied and have proven efficacy.
Pharmacotherapy (Antidepressants)
The treatment guidelines recommend that, in addition to psychotherapy, antidepressants be used for moderate and severe depression. The principle of action of modern antidepressants is mainly based on supporting and increasing the concentration of neurotransmitters serotonin, norepinephrine and dopamine at the junctions of neurons in the brain. Modern antidepressants have a specific effect on certain components of these transmitter systems. Depending on the antidepressant used, the target sites of action differ, which is why modern antidepressants often have different effects and side effect profiles that can be used to advantage in therapy. Thus, some antidepressants additionally have a sleep-promoting or analgesic effect, or also improve cognitive functions.
Light therapy
This almost side-effect-free therapy has proven to be effective not only in the treatment of winter depression, but in other types of depression. The earlier in the course of the disease, morning light therapy takes place, the better is usually the treatment success. In typical recurrent depression in autumn and winter, the treatment can also be used preventively.
Sleep deprivation
A night without sleep improves the mood. This sounds strange at first, as many depressed patients already suffer from sleep disorders, but even a partial sleep deprivation starting at about 1 o’clock in the morning is antidepressant. That means you go to bed at your usual time and wake up at 1 o’clock in the morning. It is important that during the rest of the night and throughout the following day you must not fall asleep, not even for a short time. This therapy can bridge the time to the effect of an antidepressant and is usually performed in a therapeutically-assisted group, since the sole implementation is very difficult.
Electroconvulsive therapy (ECT)
ECT is used to treat treatment-resistant depression and major depressive episodes – usually when other therapies have failed or have not been sufficiently effective. The treatment is considered effective and the onset usually takes place quickly. The treatment principle is a therapeutic seizure in the brain that is gently triggered in short anesthesia and muscle relaxation. During this approximately one-minute event, the patient is anesthetically monitored.
Pulsed Electromagnetic fields (PEMF)
PEMFs have been shown to have beneficial effects on anxiety and depression in both chronic and acute forms. While there is considerable research into the benefits of treating depression, the exact mechanisms of action, at both high and low intensities, are still not fully understood.
However, recent science suggests that transcranial magnetic stimulation (TMS) can synchronize the electrical activity of the brain, from the individual brain cell to the connected neuronal networks. Brain development and learning processes are based on the synchronization of vibrations (oscillations) of the various networks in brain activity. The ability of the brain to adapt to new demands is called neuroplasticity. It is believed that the synchronization of neuronal oscillations helps neuroplasticity, whether achieved pharmacologically or neuromodulatory, with PEMFs or brainwave entrainment devices 1.
It is not clear exactly how low-intensity PEMF stimulation works to relieve mood problems. However, it is believed that their mode of action differs from high intensity transcranial magnetic stimulation or electrical brain stimulation. Lower intensity systems are believed to cause neurons to vibrate in the frequency of the applied PEMF. This stimulation affects the electrical activity of neurons, which alter the neural network and affect the areas of mood control in the brain 2.
Electromagnetic fields also appear to affect glucose metabolism of brain regions involved in depression and anxiety and the release of various neurotransmitters, including BDNF. These regional changes have been extensively captured in the brain by neuroscientists.
After finding that functional Magnetic Resonance Imaging (fMRI) improved symptoms of bipolar depression (BPD) patients, Harvard Medical School conducted a study with a low-intensity PEMF device. They used a 1000 Hz (1 kHz) square wave / trapezoidal wave signal with 20 Gauss (2 mT) of maximum field intensity to see if it could help those affected faster than traditional treatments. In this double-blind, sham-controlled study, significant improvement in mood was greater than 10% in 41 patients with BPD and 22 with major depression (MDD) with only one 20-minute treatment. All patients received stable medication at least 6 weeks prior to PEMF treatment and had a recent episode of depression. Other findings included significant improvements in guilt, work ability, life interest, and some aspects of anxiety. In other words, based on these results, this PEMF signal indicates to be useful for a number of forms of depression and anxiety.
1. Wang L, Yang J, et al. Modulation of Low-Frequency Pulsed Magnetic Field on Hippocampal Neural Oscillation in Depression Rats. Conf Proc IEEE Eng Med Biol Soc. 2018 Jul; 2018:259-262.
2. Leuchter AF, Hunter AM, et alx. Rhythms and blues: modulation of oscillatory synchrony and the mechanism of action of antidepressant treatments. Ann N y Acad Sci. 2015 May; 1344:78-91.
In patients with treatment-resistant depression, a low-intensity transcranial PEMF (T-PEMF) was used in combination with antidepressants. In a controlled double-blind study, active or sham-T-PEMF application was compared for five weeks in patients with treatment-resistant depression. The antidepressant treatment against which patients were resistant was unchanged 4 weeks before and during the study period. The study participants were assessed weekly. The 9 Gauss (0.9 mT) 50 Hz T-PEMF and square wave was delivered via a helmet containing seven separate spin coils that were located above the skull and created an electric field in the brain tissue, much weaker than that in high intensity transcranial magnetic stimulation. The active T-PEMF group had a significantly better result than the control group with sham T-PEMF, with onset within the first weeks of therapy. The reduction on a depression rating scale was 62% 3.
In a similar home-study with the same device, it was found that the depression had disappeared by 27% after five weeks of once-daily use, and even in 73% after eight weeks 4,5. Of those treated, 52% were in remission two years later. For those who were not in remission, this could be achieved by an additional treatment. It is not yet known if even longer treatment times would bring even better results at the beginning. Many people who do not respond to treatment may have other problems, such as alcohol or drug addiction, severe physical disorders, and other psychosocial problems that need to be addressed before attempting T-PEMF treatment 2.
3. Martiny K, Lunde M, et al. Transcranial low voltage pulsed electromagnetic fields in patients with treatment-resistant depression. Biol Psychiatry 2010, 68:163-169.
4. Bech P, Lindberg L, et al. 2-year follow-up study of patients participating in our transcranial pulsating electromagnetic fields (T-PEMF) augmentation in treatment-resistant depression. Acta Neuropsychiatrica 2015.
5. Straaso B, Lauritzen L, et al. Dose-remission of pulsating electromagnetic fields as augmentation in therapy-resistant depression: a randomized, double-blind controlled study. Acta Neuropsychiatrica 2014.
Other
In parallel with these forms of therapy, individually designed accompanying measures can be very helpful, which in many different ways promote the perception of body sensation and stress management, e.g. Biofeedback, progressive muscle relaxation, stress management, massage, acupuncture, meditation, tai-chi etc.
SUMMARY
In summary, the use of magnetic stimulation in the treatment of depression is an exciting and so far, very promising treatment method, which does not replace the well-established therapy of psychotherapy and possible pharmacotherapy, but can complement it positively and is almost free of side effects. The exact mechanisms of action in both low-intensity PEMFs and high-intensity TMS have yet to be determined, but their utility has been demonstrated in numerous studies. Further research in this field is needed.
Research online for yourself about PEMF therapy, and learn more about all of the studies that have been conducted on improving overall health by PEMF therapy.
Contact us anytime, we are just a Phone Call away to assist you! Or simply just WhatsApp us now.